Over the years, I’ve treated countless patients struggling with acne — from young teenagers to adults in their forties. And I’ve realized one thing: acne is not just a skin problem. It affects your confidence, your mood, and how you see yourself in the mirror every day. In this guide, I’ll break down the acne causes, symptoms, and treatment options that actually work — based on both science and real clinical experience.
I have seen patients cancel events, skip interviews, or avoid social situations just because of a pimple breakout. Some even walk into my clinic with makeup on, not because they want to look good — but because they want to hide. That is how deep acne can go.
I understand how frustrating and emotionally exhausting it can be. You try every face wash, every cream, follow all the internet tips, and yet the breakouts keep coming. If this sounds like you, I want you to know — it is not your fault, and it is definitely treatable.
In this guide, I will walk you through acne in a way most people do not talk about — honestly, medically, and with real solutions.
You will learn:
- What exactly acne is and how it differs from normal pimples.
- The real causes behind breakouts (not just myths).
- Different types of acne and how to identify them.
- Why some people suddenly start breaking out despite healthy habits.
- Proven ways to treat acne — naturally, medically, and professionally.
- When acne could be a sign of something deeper like hormonal imbalance or a medical condition.
- How to build a daily skincare routine that actually works.
- And most importantly, how to prevent pimples from coming back again and again.
This is not just about creams or prescriptions. It is about understanding your skin and treating acne from the root.
Let us begin by answering the most basic — and most misunderstood — question:
What is acne, really?
What Is Acne?

Acne is one of the most misunderstood skin conditions I see in my practice. Many patients come to me saying, “I just keep getting these stubborn pimples.” But what they often do not realize is that acne is more than just the occasional spot. It is a deeper issue happening beneath your skin’s surface.
What Really Happens Under Your Skin?
Your skin has tiny openings called pores, and each pore is connected to an oil gland and a hair follicle. These oil glands produce sebum, which keeps your skin moisturized.
But sometimes, things go wrong.
- Dead skin cells do not shed properly
- Excess oil clogs the pores
- Bacteria start growing inside that clogged pore
The result? Inflammation, redness, pus, and sometimes painful lumps — this entire chain reaction is what we call acne.
Acne vs Pimples – Is There a Difference?
Yes, and this is important to understand — not every pimple means you have acne.
Here is how I explain the difference to my patients:
| Feature | Pimples | Acne |
| What it is | A single or occasional spot | A recurring skin condition |
| Caused by | Blocked pore or minor infection | Hormonal imbalance, oil production, bacteria, and inflammation |
| Severity | Usually mild | Can be mild, moderate, or severe |
| How it appears | Small red or pus-filled bump | Multiple breakouts: blackheads, whiteheads, cysts, etc. |
| Treatment | Often treated with basic creams or home care | May need long-term medical treatment and skin management |
Think of pimples as symptoms. Acne is the condition.
How Does Acne Actually Form?
Here is a simple breakdown of the process:
- Clogged pores: Dead skin cells and sebum block a hair follicle
- Bacterial growth: A bacteria called Cutibacterium acnes (formerly Propionibacterium acnes) multiplies inside
- Inflammation: The area becomes red, swollen, and painful
- Lesion develops: You get blackheads, whiteheads, pustules, or even deep cysts
The type of acne you develop depends on how deep and inflamed the clogged pore becomes. Some breakouts stay near the surface, while others grow deeper and hurt more.
In the next section, I will help you identify the different types of acne — so you can understand exactly what is happening on your skin and how to treat it right.
Types of Acne and How to Identify Them
One of the first things I ask my patients is: “What does your acne look like?”
That is because different types of acne require different treatments. What works for blackheads might make cystic acne worse.
So, let us break it down — simply and clearly — so you can figure out what you are really dealing with.
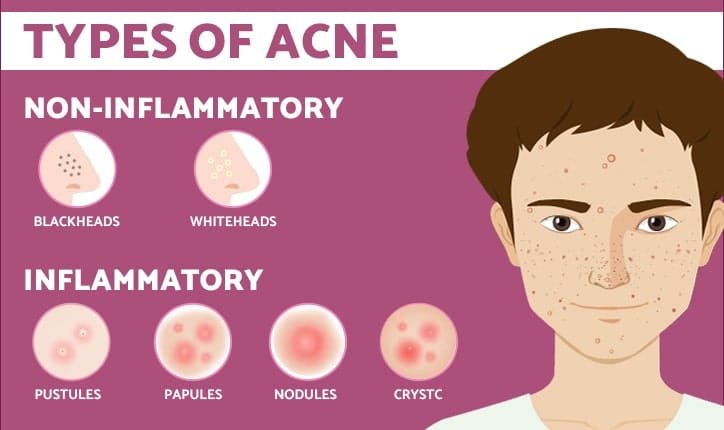
Non-Inflammatory Acne
These types usually do not hurt or feel swollen. They sit on the surface of your skin and often go unnoticed until they multiply.
1. Blackheads
- Open pores filled with oil and dead skin
- The dark color is not dirt — it is the sebum reacting with air
- Common around the nose, chin, and forehead
2. Whiteheads
- Closed clogged pores just beneath the skin
- Appear as small white or skin-colored bumps
- No redness or swelling
These are the mildest forms of acne and respond well to gentle skincare and exfoliation.
Inflammatory Acne
Now we are getting into acne that is red, swollen, and often painful. This is where infections and deeper inflammation come into play.
3. Papules
- Small red or pink bumps
- No pus at the top
- Often sensitive to touch
4. Pustules
- Look similar to papules but filled with pus
- Have a white or yellow tip
- Red at the base and may feel tender
5. Nodules
- Large, solid, and painful lumps
- Develop deep under the skin
- Often last longer and leave marks
6. Cystic Acne
- The most severe type
- Soft, pus-filled bumps deep beneath the skin
- Often leave scars and need medical intervention
Quick Comparison Table
| Type | Appearance | Pain Level | Depth | Risk of Scarring |
| Blackheads | Small black dots | None | Surface | Low |
| Whiteheads | White or skin-colored bumps | None | Surface | Low |
| Papules | Red, raised bumps | Mild | Moderate | Moderate |
| Pustules | Red with white top | Mild to moderate | Moderate | Moderate |
| Nodules | Large, solid lumps | High | Deep | High |
| Cysts | Large, soft, pus-filled lumps | Very high | Very deep | Very high |
Knowing your acne type is the first step toward choosing the right treatment plan. In the next section, I’ll explain how acne is graded based on severity — because not all acne is equally intense, even if it feels that way.
Grades of Acne Severity

(And How You Can Assess It at Home)
When patients come to me for acne concerns, one of the first things I evaluate is the severity of their condition. Why? Because the right treatment depends not only on the type of acne — but also on how widespread and inflamed it is.
Even if you’re not a medical professional, you can get a good idea of where your acne falls by understanding the grading system. Acne is generally classified into three levels: mild, moderate, and severe.
Let me walk you through each one.
Grade 1: Mild Acne
This is the most common type I see in younger patients or those just starting to break out.
What it looks like:
- A few whiteheads or blackheads
- Occasional small red pimples
- Mostly concentrated on the T-zone (forehead, nose, chin)
- No pain, swelling, or scarring
What it feels like:
Your skin might feel oily or bumpy in certain areas but not sensitive or inflamed.
Home care tip:
Mild acne often improves with a basic routine — gentle cleanser, salicylic acid, and oil-free skincare.
Grade 2: Moderate Acne
This level needs more care. It’s no longer just surface-level congestion — inflammation has started to take over.
What it looks like:
- More frequent breakouts
- Visible whiteheads, blackheads, papules, and pustules
- May spread to cheeks, jawline, and upper back
- Some pimples leave behind red or dark marks
What it feels like:
Skin may feel tender in breakout areas. You might notice a breakout nearly every week.
Home care tip:
Over-the-counter options may no longer work. You may need a mix of topical and oral medications under medical guidance.
Grade 3: Severe Acne
This is when acne becomes painful, widespread, and emotionally distressing.
What it looks like:
- Deep, painful cysts or nodules
- Inflammation across large areas: face, chest, back
- Lesions take weeks to heal
- High chance of permanent scarring
What it feels like:
Your skin feels sore, even when not touching it. New cysts form before older ones have healed.
Home care tip:
Please don’t wait. This type of acne almost always requires medical intervention — prescription medicines, advanced peels, laser, or scar-reduction therapies.
Self-Check Table: What Grade Is Your Acne?
| Grade | Main Symptoms | Pain Level | Scarring Risk | Suggested Action |
| Mild | Few blackheads, tiny pimples | None | Low | Basic skincare at home |
| Moderate | Frequent breakouts, red bumps | Mild to Moderate | Medium | Medical advice may be needed |
| Severe | Painful cysts, nodules, scarring | High | High | Immediate professional care |
Knowing your acne grade is the foundation for finding the right treatment. Treating severe acne with just face wash or ignoring mild acne until it worsens — both are common mistakes I see.
In the next section, I’ll help you understand exactly what causes acne — so we can treat it not just from the outside, but at the root level.
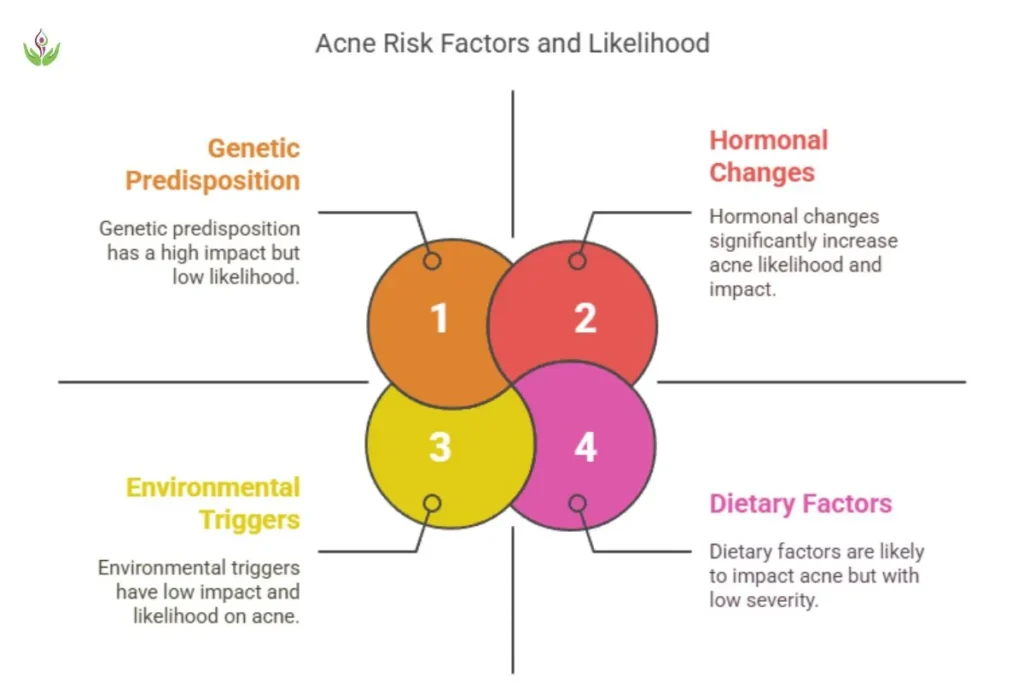
What Causes Acne?

(And Why It’s Not Just About Oily Skin)
Let me tell you something I often share with my patients — acne is not caused by poor hygiene or eating one piece of chocolate. That is a myth.
Acne is a complex skin condition that usually results from multiple internal and external factors. Understanding these causes is key to building a treatment that actually works.
Internal Causes of Acne
These are factors inside your body — things you often cannot control completely, but can manage with the right help.
1. Hormonal Imbalances
- One of the biggest culprits, especially in teenagers, women with PCOD, and adults with irregular cycles
- Androgens (male hormones) increase oil production, which clogs pores
- This is why women often get chin or jawline acne during periods or pregnancy
2. Excess Sebum Production
- Your oil glands work overtime, flooding your skin with more oil than it needs
- This creates the perfect trap for dead skin and bacteria
3. Dead Skin Cell Build-Up
- When dead cells do not shed properly, they block the pores
- This blockage mixes with oil and leads to breakouts
4. Bacterial Growth (C. acnes)
- A natural skin bacteria becomes aggressive inside clogged pores
- This triggers inflammation and pus-filled pimples
5. Genetics
- If your parents had acne, your chances of getting it increase
- Some people naturally produce more oil or have more reactive skin
External Causes and Triggers
Sometimes, everyday habits or environmental changes can worsen acne — even if the root issue is internal.
1. Stress
- It does not directly cause acne, but it can worsen it
- Stress boosts cortisol and androgens, leading to oilier skin and flare-ups
2. Skincare Products
- Heavy, greasy, or comedogenic products block pores
- Over-cleansing or using harsh products can strip the skin and trigger rebound oiliness
3. Diet and High-Glycemic Foods
- Sugar, white bread, fried snacks, and processed foods can spike insulin
- This affects hormone levels and may lead to more acne
- Dairy products — especially skim milk — have also been linked to breakouts in some people
4. Environmental Pollution
- Dust, smog, and sweat mix with skin oil, clogging pores even more
- Pollution may also trigger inflammation and oxidative stress on your skin
Common Myths — Debunked
Let me set the record straight:
- Chocolate doesn’t cause acne. Excess sugar might, but not cocoa.
- Masturbation has no link to acne. It is a hormonal myth.
- Poor hygiene is not the root cause. In fact, over-washing your face can make acne worse.
- Greasy food is not the main villain. But diets high in sugar and processed carbs can contribute.
Summary: Why You Might Be Breaking Out
| Root Cause | Triggers/Aggravators |
| Hormonal Imbalance | Menstrual cycle, PCOD, pregnancy, puberty |
| Excess Oil & Dead Skin | Genetics, harsh products, poor exfoliation |
| Bacterial Infection | Clogged pores, untreated acne, picking pimples |
| Lifestyle & Environment | Stress, diet, pollution, product misuse |
In the next section, I’ll explain specific medical conditions that often hide behind recurring or sudden acne — especially in adults. If your acne keeps coming back no matter what, this might be the missing link.
Medical Conditions That Cause Acne

(When Breakouts Are a Symptom, Not the Main Problem)
Many patients come to me after trying every possible cream, face wash, or home remedy — but their acne keeps returning. In such cases, I always ask a crucial question:
“Have you checked if your acne is linked to an internal health issue?”
Sometimes, acne is not just a skin condition. It can be a sign of an underlying medical problem, especially when it is sudden, painful, or resistant to regular treatments.
1. Hormonal Disorders
Hormonal imbalances are one of the most common root causes of adult and cystic acne — especially in women.
Polycystic Ovary Syndrome (PCOD/PCOS)
- High androgen levels increase sebum production
- Causes acne on the jawline, chin, and cheeks
- Often accompanied by irregular periods, weight gain, and facial hair
Thyroid Disorders
- Both hypothyroidism and hyperthyroidism can cause hormonal shifts
- These affect skin hydration, oil balance, and inflammation
Cushing’s Syndrome
- A rare condition caused by high cortisol levels
- Leads to facial acne, thinning skin, and excessive body hair
Acromegaly
- Excess growth hormone leads to enlarged pores and thick, oily skin
- Results in stubborn acne that does not respond to regular care
2. Genetic Syndromes and Immune Conditions
Some rare medical conditions also involve acne as one of their symptoms.
Apert Syndrome
- A genetic disorder that affects skin and bone development
- Severe acne can be a visible symptom
PAPA Syndrome
(Pyogenic Arthritis, Pyoderma Gangrenosum, and Acne)
- An inherited autoinflammatory disorder
- Causes painful nodulocystic acne along with joint pain and ulcers
Behçet’s Syndrome
- Autoimmune condition with symptoms like skin lesions, ulcers, and acne-like rashes
3. Weak Immune System and Chronic Infections
You might be surprised to know — a weak immune system can also make acne worse.
- When immunity is low, your skin cannot fight bacterial infections properly
- Stress, fatigue, poor diet, or ongoing infections can reduce skin defense
- This is why breakouts often worsen during or after fever, cold, or illness
When Should You Suspect a Medical Cause?
Here are some red flags that suggest your acne may be linked to an internal health condition:
- Acne appears suddenly in adulthood (age 25+)
- Pimples are deep, painful, and concentrated on the lower face or jaw
- Acne does not respond to standard treatments
- You have irregular periods, hair loss, or unexpected weight changes
- There is a family history of PCOD or endocrine disorders
- Acne appears along with fatigue, body pain, or other unexplained symptoms
If any of these sound familiar, I recommend getting blood tests or a hormone panel done. In many such cases, treating the underlying condition helps resolve the acne much faster and more permanently.
In the next section, I will explain why acne sometimes flares up suddenly, even in people who usually have clear skin.
7. What Causes Sudden Acne Breakouts?

Let me ask you something — have you ever woken up with unexpected pimples, even though your skin had been fine for weeks or months?
You are not alone.
As a cosmetic surgeon, I often meet adults who say, “I never had acne in my teenage years. Why am I breaking out now?”
The truth is, sudden acne breakouts are becoming increasingly common, especially in people over 25. And no — it is not just because of oily food or dirty pillows.
Let’s break down a few real reasons why your skin might be reacting out of nowhere.
A Real Example from My Clinic
Not long ago, I treated a 34-year-old working professional. She had flawless skin most of her life. But within two months of switching jobs, taking whey protein shakes, and skipping meals, she developed painful breakouts along her jawline and chin.
Her question: “Why now?”
My answer: “Your skin is reflecting what your body is trying to balance inside.”
Let me walk you through the most common reasons your skin can suddenly react, even if it has never given you trouble before.
Hormonal Swings You Didn’t See Coming
Whether you are a woman in your 20s or a man in your 40s, your hormones can surprise you.
- Women often experience breakouts just before their periods, during ovulation, or after stopping birth control.
- Pregnancy, postpartum shifts, or even menopause can shake up your skin’s oil production.
- In men, testosterone spikes from workouts, stress, or supplements can also trigger flare-ups.
If your pimples are showing up on your jawline, chin, or lower cheeks — hormones might be the root.
Stress — The Silent Skin Disruptor
You may not link stress to acne right away. But your body does.
When you are anxious, sleep-deprived, or mentally exhausted, your body releases cortisol — a hormone that pushes your oil glands into overdrive.
No surprise then, that your skin might erupt just before a big presentation, a major life event, or during emotional burnout.
Food and Skin — A Subtle but Powerful Connection
Here is something many people overlook: your diet may not directly cause acne, but it often fuels it.
- High-glycemic foods like white rice, bread, sugar, and fried snacks spike your insulin — which affects oil production
- Dairy, especially low-fat milk and whey protein, has been linked to adult acne in several studies
- Sudden diet changes — like switching to a high-protein supplement or skipping meals — can shock your system
If your skin changed after your diet did, it is worth looking at what’s on your plate.
Your Medications Might Be Messing With Your Skin
This one surprises a lot of patients.
Certain medicines are known to trigger acne as a side effect. For instance:
- Hormonal pills and IUDs
- Steroids — taken for asthma, allergies, or gym gains
- Antidepressants or antiepileptics
- Biotin or multivitamins in high doses
It does not mean you have to stop them — but it helps to inform your doctor and adjust your skincare accordingly.
Are You Sleeping Well?
It sounds simple, but if you are not sleeping enough or your sleep-wake cycle is irregular, your skin pays the price. Nighttime is when your body repairs inflammation — including acne.
Interrupted sleep = prolonged healing = new breakouts.
Health Issues That Show Up on Your Skin First
Lastly, if your acne feels intense, painful, and out of character — your body might be trying to signal something deeper.
Conditions like PCOD, thyroid imbalance, insulin resistance, or even high cortisol (as seen in Cushing’s syndrome) can first show symptoms through skin changes.
So, if breakouts come with irregular periods, hair thinning, fatigue, or sudden weight gain — please get checked. It is better to be proactive than to wait.
Bottom Line?
If your acne showed up suddenly — without changing your skincare — something inside you has likely shifted. It could be stress, hormones, food, medication, or even an undiagnosed medical issue.
Instead of panicking or jumping from product to product, try asking:
“What changed in my life just before this started?”
That answer often leads you to the real trigger.
In the next part, we will explore who is naturally more prone to acne and what factors increase your risk — even if your skin was clear before.
Risk Factors That Increase Acne
(Why Some People Break Out More Than Others)
You might wonder — “Why do I get acne while my friend with the same lifestyle has perfectly clear skin?”
The truth is, acne is not just about skincare habits or diet. It is about how your skin responds to certain internal and external triggers. That response is shaped by your body’s chemistry, your genetics, and your environment.
Below are the key risk factors I’ve seen consistently across hundreds of patients — men and women alike.
1. Your Genes May Be Guiding Your Skin
If acne runs in your family, your skin might naturally produce more oil, shed dead cells slower, or react more aggressively to bacteria.
- You may break out more often.
- Acne might be more severe.
- You’re more likely to develop post-acne marks or scars.
Tip: Early treatment helps reduce long-term impact if you’re genetically prone.
2. Age and Hormonal Life Stages
Acne is most common during puberty, but it doesn’t end there. I often treat:
- Teens with classic forehead and nose breakouts.
- Women in their 30s with jawline acne related to PCOD or stress.
- Men in their 40s who develop cystic acne due to testosterone fluctuations or supplements.
Even perimenopause and menopause can bring on hormonal skin shifts.
3. Product Overload or Misuse
Ironically, trying too many skincare products can harm more than help.
- Thick moisturizers or silicone-based primers may clog pores.
- Harsh scrubs or alcohol-based toners can damage the skin barrier.
- Frequent switching of products confuses your skin and worsens sensitivity.
Stick to a consistent, non-comedogenic routine suited to your skin type.
4. Skin Friction and Pressure (Yes, It Matters)
You might not realize this — but even mechanical irritation can trigger acne.
Here’s what I often see:
- Acne flares under tight helmets, face masks, collars, or headbands.
- Shoulder or back acne worsens in people wearing heavy backpacks daily.
- Frequent phone-to-face contact can cause breakouts on one cheek.
This is called acne mechanica, and it is surprisingly common.
5. Diet Rich in High-Glycemic Foods
Not everyone reacts to food, but if you do — sugar, white carbs, and dairy can cause inflammation and hormonal shifts.
You are at higher risk if:
- You consume a lot of sweets, cold drinks, or processed snacks.
- You use protein powders, especially whey.
- You eat fewer fresh fruits, veggies, or omega-3 rich foods.
6. Environmental and Lifestyle Triggers
Pollution, sweating, poor air quality, or dirty pillowcases — all add up.
Also, your risk rises if you:
- Smoke or consume alcohol regularly.
- Are sleep-deprived or under constant work pressure.
- Touch your face frequently or skip makeup removal at night.
Who Is More Likely to Develop Acne?
| High-Risk Profile | Why |
| Teenagers and young adults | Hormonal surge, oil gland activity |
| Women with PCOD or hormonal imbalance | Androgen excess and menstrual shifts |
| Gym-goers using whey protein or steroids | Dietary triggers and hormonal load |
| Individuals with oily skin and family history | Genetic and sebum-related factors |
| People exposed to stress and poor sleep | Cortisol imbalance and poor healing |
| Urban dwellers exposed to daily pollution | Skin barrier damage and oxidative stress |
Areas of the Body Where Acne Can Appear
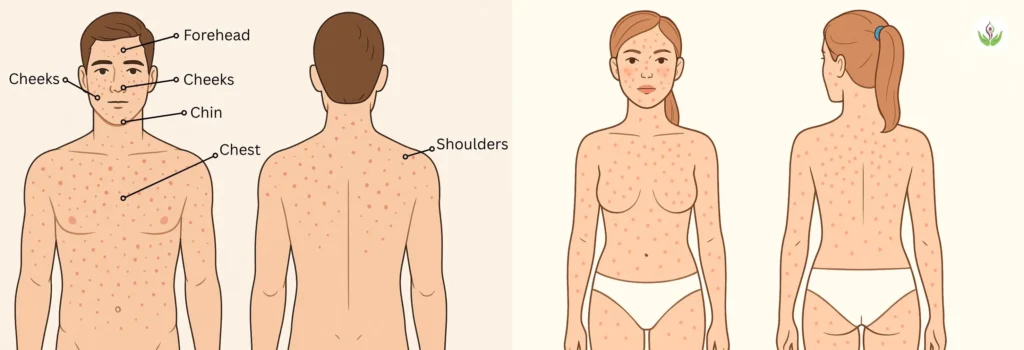
(And What Each Location Might Be Telling You)
When patients visit me for acne treatment, most are focused on their face — which makes sense. It is the most visible part of our skin. But what surprises many of them is that acne can affect several other areas of the body too.
In fact, one of the first things I observe during a consultation is where the breakouts are happening. That location often reveals a lot about the root cause.
Let me walk you through what I’ve learned over the years.
Face — The Usual Suspect
Most people break out on the face, especially the T-zone — the forehead, nose, and chin.
- If I see forehead acne, I usually ask about scalp health. Dandruff or hair oil buildup is often the hidden culprit.
- Nose acne often comes from enlarged pores, excessive oil, or pollution buildup.
- But when I see acne around the jawline or chin, especially in women, I immediately think of hormones. PCOD, stress, or cycle-related changes often show up there.
- Acne on the cheeks? I always ask about phone hygiene and pillowcases — you would be shocked how many people forget to change them regularly.
Back — Common in Gym-Goers and Teenagers
Back acne — or what many call “bacne” — is something I treat often, especially in active individuals.
The back has large sebaceous glands, so it produces more oil. Add sweat, friction from backpacks, and synthetic gym wear — and you have the perfect environment for clogged pores.
Many of my patients with back acne tell me they shower late after working out. That small delay alone can make a huge difference.
Chest — A Sweat and Fabric Issue
The chest is another common zone I examine.
Tight or synthetic clothing, sports bras, and excessive sweating all play a role here. In Delhi’s humid summers, chest acne often worsens — especially if you’re outdoors a lot or work in heat-prone environments.
Sometimes, the skincare products you’re using for your face trickle down and clog pores on your chest too.
Shoulders and Upper Arms
If you carry a laptop bag or wear tight straps every day, your shoulders may be at risk for acne — or something that looks very similar.
In this area, it’s not always acne. Many people actually have follicular keratosis — rough bumps due to clogged hair follicles — which can be mistaken for breakouts.
Buttocks and Thighs
Let me clarify — this is usually not acne. What shows up on the buttocks is often folliculitis, which mimics acne but is technically an infection or irritation of the hair follicle.
In my experience, this tends to affect people who wear tight jeans or sit for long hours in warm environments. It’s common but underreported due to the area being hidden and sensitive.
My Observational Map of Acne-Prone Zones
| Area | What I Usually Find |
| Forehead | Oil buildup, dandruff, or heavy hair products |
| Jawline/Chin | Hormonal issues, PCOD, stress-related acne |
| Back | Post-gym sweat, friction, synthetic clothing |
| Chest | Heat rash, product transfer, tight fabrics |
| Shoulders/Arms | Strap pressure, keratosis pilaris, sweat |
| Buttocks/Thighs | Folliculitis from sitting or tight clothing |
When you pay attention to where acne shows up, you get one step closer to understanding why it is happening in the first place. In my practice, that’s often the turning point in choosing the right treatment plan.
Next, let’s talk about something that’s rarely discussed — can acne be a sign of something more serious? The answer might surprise you.
Can Acne Be a Sign of Serious Illness?
(And When You Should Stop Treating It on Your Own)
I want to be very honest here — most acne is not dangerous. It is frustrating, yes. It affects your confidence, your daily routine, and sometimes even your mental health. But in most cases, it is a treatable skin condition, not a sign of something serious.
That said, I have seen some cases where acne is actually a symptom of an underlying medical problem.
Let me share what I have learned over the years, and when I start to dig deeper as a cosmetic surgeon.
When Acne Might Mean More Than Just Acne
If someone comes to me with deep, painful breakouts — especially if they start suddenly or resist every kind of treatment — I start asking questions about their overall health.
Why? Because in some cases, the skin is just the messenger.
Excess Hormones = Excess Acne
One of the biggest red flags is hormonal imbalance. Androgens (male hormones) increase oil production. When these are elevated — due to PCOD, adrenal issues, or other endocrine disorders — the skin reacts.
In women, I often see:
- Irregular periods
- Chin or jawline acne
- Facial hair or thinning scalp hair
- Sudden weight gain
In such cases, I usually recommend a hormone panel and ultrasound. Treating the root hormone issue often clears the skin too.
Thyroid, Adrenal & Other Gland Issues
Low thyroid (hypothyroidism) can make the skin sluggish and oilier.
Cortisol excess (as seen in Cushing’s Syndrome) can lead to facial acne, skin thinning, and mood changes.
Once, I had a patient who struggled with persistent acne and unexplained fatigue. Blood tests revealed a thyroid imbalance she had no idea about. Treating that condition helped her skin improve within weeks.
Rare but Important Conditions
There are also rare autoimmune or genetic conditions like:
- PAPA Syndrome (which includes acne, arthritis, and skin ulcers)
- Apert Syndrome
- Behçet’s disease
These are not common — but when acne is unusually severe, painful, or spreads with ulcers or joint pain, I never ignore the possibility.
Mental Health and Immune Suppression
Stress does more than make you tired — it suppresses your immune system.
I’ve observed patients during exam season or life transitions break out repeatedly. Their body is in overdrive, their sleep is disrupted, and immunity dips. The skin reflects all of it.
Chronic infections or a weak immune response can also reduce your skin’s ability to fight off acne-causing bacteria.
When You Should Definitely See a Doctor
You don’t need to panic, but here’s when I recommend getting evaluated beyond just skincare:
- Acne appeared suddenly after age 25
- You’ve tried multiple treatments with zero improvement
- Breakouts are painful, leave marks, or keep recurring in the same spots
- Acne is accompanied by irregular periods, hair loss, fatigue, or weight shifts
- You have a family history of PCOD, thyroid, or autoimmune disease
- You feel emotionally burnt out, anxious, or chronically sleep-deprived
- Your skin is not being difficult — it is trying to communicate.
In the next section, I’ll explain how your immune system plays a role in acne development, especially in people who fall sick often or heal slowly.
Is Acne Linked to a Weak Immune System?
(And Why You Break Out More When You’re Run Down)
This is a question many of my patients never think to ask — but it often explains a lot:
“Is my acne somehow related to my immune system?”
In my experience, the answer is yes — in many cases, your body’s ability to fight infection and heal inflammation directly influences how your skin behaves.
Let me explain.
Why Acne Gets Worse When You’re Sick or Stressed
Have you noticed how your skin tends to break out right after you’ve had a fever, flu, or even a few nights of poor sleep?
That is not a coincidence.
When your immune system is weakened — whether from illness, stress, lack of sleep, or poor nutrition — your skin becomes more vulnerable to bacterial overgrowth and inflammation.
The acne-causing bacteria (Cutibacterium acnes) naturally lives on your skin. A strong immune system usually keeps it in check. But when your defenses are low, it multiplies quickly — leading to deeper, more painful breakouts.
Chronic Stress = Suppressed Immunity = More Acne
Here’s what I often see:
Students before exams. Professionals in high-pressure jobs. New mothers who are sleep-deprived.
They come in with red, inflamed skin and say, “I haven’t changed anything — but my skin’s gone wild.”
That is cortisol in action. Your stress hormone not only increases oil production but also slows your skin’s healing response. The result? Acne that lasts longer, spreads faster, and heals slower.
Poor Nutrition and Gut Health Also Matter
Your immune system starts in your gut.
If you’re eating too much processed food, not getting enough vitamins, or dealing with digestive issues — your immune response weakens. That shows up on your skin too.
I’ve seen patients with frequent colds, bloating, or gut inflammation also report persistent acne. Once we support their digestion and nutrition, their skin often improves dramatically.
The Inflammation-Immunity-Acne Triangle
Here is how I explain it in simple terms:
- Weak immunity leads to
- Uncontrolled inflammation, which triggers
- Severe or cystic acne
Your skin is not just reacting to clogged pores. It is reacting to what is happening inside your immune and hormonal systems.
Signs Your Acne Might Be Linked to a Weakened Immune System
You do not need a lab test to start connecting the dots. Ask yourself:
- Do you get sick often or take longer to recover?
- Do your breakouts flare up after stress or poor sleep?
- Does your acne worsen when your digestion is off?
- Are your pimples deep, painful, and slow to heal?
If yes, your immune system might be struggling — and your skin is showing it first.
In the next section, I will walk you through how I help patients identify their specific acne type — because understanding what kind you have is essential before starting any treatment.
How to Diagnose Your Acne Type
(A Step-by-Step Guide to Understanding What You’re Dealing With)
One of the biggest mistakes I see people make is treating acne without knowing what kind they actually have.
I often ask my patients during the first visit, “What does your acne look and feel like?”
And most respond with, “Just pimples.”
But here’s the truth — not all pimples are the same. Some sit on the surface. Some go deep. Some are inflamed. Others are not. And each type needs a different approach.
Let me help you figure out your acne type — right now, from home.
Step 1: Take a Close Look in the Mirror (In Natural Light)
Use a clean mirror and good lighting. Gently inspect your face, back, chest, or wherever breakouts are occurring. Do not squeeze anything — just observe.
Ask yourself:
- Are the bumps black, white, red, or skin-colored?
- Do they hurt when touched?
- Are they deep or close to the surface?
- Is there pus or just redness?
Your answers will guide the next step.
Step 2: Match Your Breakouts with These Acne Types
Here’s a simplified guide I use during consultations:
| Acne Type | How It Looks | How It Feels | Depth |
| Blackheads | Small dark dots (open pores) | Not painful | Surface |
| Whiteheads | Tiny white or skin-colored bumps | Not painful | Just below skin |
| Papules | Small red bumps without pus | Slightly tender | Mid-level |
| Pustules | Red bumps with white or yellow pus | Tender and sore | Mid-level |
| Nodules | Large, solid, painful lumps | Deep and painful | Deep in skin |
| Cysts | Big, soft, pus-filled swellings | Very painful and inflamed | Very deep |
Once you identify the type, you can better understand what treatment will work — and what might make it worse.
Step 3: Observe Patterns Over Time
Ask yourself:
- Do you break out more before your period or after stress?
- Is it always on the same part of your face or body?
- Are the spots large and few or small and many?
These patterns tell me — and will tell you — whether your acne is hormonal, bacterial, frictional, or inflammatory.
Step 4: Avoid This Common Mistake
Do not treat every bump the same.
For example:
- Scrubbing a whitehead can inflame it
- Using oil-based creams on pustules can trap bacteria
- Picking a cyst can cause permanent scarring
That is why identifying your acne before treating it is not just helpful — it’s essential.
When Should You Let a Doctor Diagnose It?
If you’re unsure even after self-checking — or if your acne keeps getting worse — I always recommend a professional diagnosis. Sometimes, what looks like acne could actually be:
- Fungal infections
- Rosacea
- Folliculitis
- Allergic skin reactions
A simple in-clinic examination (sometimes with a dermatoscope) can make all the difference.
In the next section, I’ll share exactly how I approach acne treatment — from natural options to advanced medical therapies — and how you can choose what’s best for your skin.
13. How Is Acne Diagnosed in a Clinic?
(What I Look for Before Starting Any Treatment)
Before recommending any acne treatment, I always begin with a detailed diagnosis. Acne is not just about what shows up on the skin — it is often a reflection of what is happening inside your body.
Here is how I usually approach it during a consultation:
1. Physical Examination
I start by closely examining your skin. I check the number, type, and distribution of acne lesions — whether they are blackheads, whiteheads, pustules, or deeper nodules. I also look for signs of post-acne marks or scarring.
2. Acne Mapping by Location
Where your acne appears tells me a lot.
- Jawline and chin: often linked to hormones.
- Forehead: sometimes linked to dandruff or hair products.
- Back or chest: may point to heat, sweat, or certain clothing habits.
This “acne map” helps guide whether we are looking at external triggers or internal imbalances.
3. Discussion About Lifestyle & Menstrual Health
If you are a woman and dealing with adult or persistent acne, I ask questions about:
- Irregular periods
- Sudden weight gain or hair growth
- Stress levels
- Sleep cycle disruptions
- Cosmetic product usage
This helps me decide if your acne could be hormonal or related to other medical conditions.
4. Hormonal Blood Tests (if needed)
For recurring or severe acne, especially in adult women, I may suggest tests like:
- Androgens (testosterone, DHEAS)
- Estrogen, LH/FSH ratio
- Prolactin or insulin levels
These help uncover hidden issues like PCOD, thyroid dysfunction, or insulin resistance.
5. Ultrasound or Endocrine Referral
If hormonal imbalance is suspected, I might refer you for a pelvic ultrasound or ask for an endocrinologist’s opinion. Acne may just be a symptom — we need to treat the root cause.
Most people try creams or face washes without knowing what type of acne they even have. But if we skip the diagnosis step, we may waste months — or even make things worse.
That is why I always recommend a proper skin analysis and, if needed, basic hormonal screening — especially if your acne is chronic, painful, or suddenly worsening.
How to Treat Acne Effectively

(What I Recommend — From Natural Remedies to Clinical Solutions)
Once my patients understand their acne type, the next question they always ask is:
“What’s the best treatment for my skin?”
The honest answer? There’s no one-size-fits-all.
In my practice, I treat each case differently — based on the type, severity, and underlying causes. Some patients respond well to home remedies. Others need prescription care. And in more stubborn cases, I use advanced treatments like lasers or chemical peels.
Let me walk you through all your options — in the same way I explain them during a real consultation.
Natural Remedies for Early or Mild Acne
These are helpful if your acne is occasional, non-inflammatory, or just starting out.
What I Recommend at Home:
- Raw honey + cinnamon mask (natural antibacterial)
- Diluted apple cider vinegar (1 part vinegar to 3 parts water) as a gentle toner
- Aloe vera gel, applied fresh or store-bought (fragrance-free)
- Cool green tea compress using a soaked cotton pad
- Tea tree oil, only in diluted form — never use it directly
These can help calm surface-level inflammation and keep pores clear — but they do not work for deep or cystic acne. If you’re struggling with breakouts that keep coming back, I’ve shared a detailed guide on how to cure acne permanently using lifestyle changes, clinical treatments, and skincare strategies.
Medical Treatments I Often Prescribe
For moderate or persistent acne, topical creams or oral medications are necessary. Self-treatment may not be enough.
Topical Options:
- Retinoids (like adapalene or tretinoin): Helps unclog pores and speed up cell turnover
- Benzoyl peroxide: Kills bacteria and reduces inflammation
- Salicylic acid (2%): Great for blackheads and oily skin
- Azelaic acid: Especially useful for sensitive or pigmented skin
- Topical antibiotics (clindamycin + benzoyl peroxide): Targets infection
These must be used carefully. I always recommend starting slowly — every alternate night — to avoid irritation.
Oral Medications (Prescription Only):
- Antibiotics (doxycycline, minocycline): For widespread bacterial acne
- Oral contraceptives: For women with hormone-related breakouts
- Spironolactone: Helps reduce androgens in adult women
- Isotretinoin (Accutane): For severe, nodular, or cystic acne that doesn’t respond to anything else
Isotretinoin is powerful — and needs close monitoring. I prescribe it only when truly necessary, and after bloodwork.
What I Check Before Prescribing:
- Skin type and sensitivity
- Hormone levels (if symptoms suggest imbalance)
- Lifestyle factors (stress, diet, hygiene)
- Previous product history (to avoid repeating what failed)
| Severity | Best Option | Where to Start |
| Mild | Natural remedies, OTC | Home care |
| Moderate | Prescription creams/tablets | Dermatologist consult |
| Severe | Isotretinoin, laser, peels | Clinic treatment |
Advanced Treatments I Use at My Clinic
If you’ve tried medications or if your acne is leaving scars, in-clinic treatments give faster, long-term results.
Procedures I Recommend:
- Chemical Peels (Glycolic, Salicylic, or TCA): Removes dead skin and clears congestion.
- Comedone Extraction: Safe manual removal of blackheads and whiteheads.
- Intralesional Steroid Injections: For fast shrinking of cysts or nodules.
- Laser Therapy (like Q-switch or Fractional CO2): Treats scars, pigmentation, and recurring inflammation.
- LED Light Therapy (Blue/Red): Kills acne bacteria and soothes redness.
I usually combine treatments for best results — for example, a peel followed by laser or LED. For gentle yet effective solutions, explore the benefits of chemical peel treatment and the top advantages of HydraFacial for acne-prone skin — both can unclog pores, reduce oil, and brighten your complexion without harsh side effects.
Acne Scar Treatments That Actually Work (At My Delhi Clinic)
If your active acne has healed but left behind pits, marks, or uneven texture, you are not alone. Acne scars can be stubborn, but they are not permanent.
At Care Well Medical Centre, I offer several advanced solutions that have helped my patients get smoother, clearer skin over time.
Here’s what works best, depending on your scar type:
- Microneedling (Collagen Induction Therapy): Great for shallow scars. It promotes collagen growth by using tiny skin pricks.
- Chemical Peels: We use controlled peels to remove dead skin and lighten pigmentation left by acne. Before opting for chemical treatments, it’s important to know how they work. Here are surprising things to know about chemical peels before booking your first session.
- PRP Therapy (Platelet-Rich Plasma): Uses your own blood’s healing properties to restore damaged skin and improve texture.
- Fractional CO2 Laser: This is highly effective for deep or pitted scars. It resurfaces your skin and boosts collagen from the inside.
- Subcision: For rolling scars or tethered scars, this treatment breaks the scar bands beneath the skin and allows smoother healing.
These are customized based on skin type, scar pattern, and how your skin reacts. For best results, I often combine treatments like PRP with microneedling or laser for deeper rejuvenation. If deep pits or permanent marks are bothering you, consider our Acne Scar Treatment in Delhi for visible skin improvement.
What Treatment Should You Start With?
If your acne is mild, start with gentle home care and over-the-counter actives.
If it’s moderate or persistent, see a doctor — even just once — to avoid trial-and-error damage.
And if it’s deep, painful, or scarring — do not delay medical care. The earlier we treat, the better your long-term outcome.
In the next section, I’ll talk about something most people overlook — your diet. What you eat can have a huge impact on your skin, and I’ll show you how to build a skin-friendly food routine.
Not Sure Which Treatment Suits You Best?
Book a personal consultation at Care Well Medical Centre, New Delhi.
Let me examine your skin and create a plan that’s just right for you.
Best Diet for Acne Prevention
(What I Recommend My Patients Eat — and Avoid)
Over the years, I have learned one thing for sure — your skin reflects what’s happening inside your body. And diet plays a major role.
Many patients ask me, “Can food really cause acne?”
My answer? It is not always the food — it’s how your body reacts to certain ingredients. Some people eat pizza and never break out. Others react after a single scoop of ice cream.
So instead of blindly cutting foods, I encourage my patients to build a balanced, anti-inflammatory diet — one that supports hormonal balance, gut health, and immunity.
Here’s what I recommend.
What to Eat for Clearer Skin
Let me start with the foods I personally rely on — and regularly suggest to my acne-prone patients.
Low-Glycemic Foods
Foods that release sugar slowly help control insulin levels, which in turn keeps oil glands in check.
- Whole grains (quinoa, oats, brown rice)
- Legumes (chickpeas, kidney beans)
- Sweet potatoes
- Most vegetables
A patient of mine reduced her acne by simply switching from white rice and noodles to millet and lentils — no medicines involved.
Omega-3 Rich Foods
Omega-3s reduce inflammation — which helps prevent red, angry breakouts.
- Fatty fish (salmon, mackerel)
- Chia seeds, flaxseeds, walnuts
- Cold-pressed flaxseed or canola oil
These not only calm acne but also help with healing and scar prevention.
Zinc-Rich Foods
Zinc helps regulate oil production and speeds up wound healing.
- Pumpkin seeds
- Cashews
- Quinoa
- Whole eggs
I often suggest a 15–30 mg daily zinc supplement for moderate acne cases, if diet alone is not enough.
Antioxidant-Rich Fruits & Veggies
Colorful foods fight oxidative stress and protect skin cells.
- Berries (blueberries, strawberries, amla)
- Spinach, kale, broccoli
- Carrots, beets, bell peppers
These work wonders when combined with enough hydration and sunlight protection.
What to Avoid (Or Limit)
Not everyone reacts to these foods — but they are frequent culprits I track in acne-prone individuals.
High Sugar, Processed Carbs
- White bread, biscuits, sugar-loaded cereals
- Cold drinks, packaged juices, candies
They spike insulin → increase androgens → trigger sebum production.
Dairy (Especially Low-Fat Milk)
Surprisingly, I have seen more breakouts in patients who consume skim milk or whey protein shakes.
It is believed that dairy may alter hormone levels — even if you’re not lactose intolerant.
If you suspect a link, try cutting dairy for 3–4 weeks and track results.
Whey Protein
This one’s huge among gym-goers. I have treated many bodybuilders and fitness enthusiasts with persistent acne linked directly to whey supplements.
I usually suggest switching to plant-based proteins (like pea, brown rice, or hemp).
Bonus Skin-Boosting Tips
- Drink at least 2.5–3 liters of water daily
- Include green tea or hibiscus tea for antioxidants
- Avoid greasy late-night meals — they mess with your digestion and your skin
My Suggested Daily Acne-Friendly Diet (Sample)
| Meal | What I Recommend |
| Morning | Warm lemon water + soaked walnuts or flaxseeds |
| Breakfast | Vegetable oats / besan chilla / boiled eggs + herbal tea |
| Lunch | Brown rice + dal + sautéed greens or mixed veg sabzi |
| Snack | Fruit + handful of pumpkin or sunflower seeds |
| Dinner | Quinoa + paneer / grilled tofu + salad or soup |
This is not a strict plan — but it’s a great starting point for clearer skin and a calmer gut.
In the next section, I’ll walk you through a simple, effective daily skincare routine — because food is half the battle. What you apply on your skin matters just as much.
Daily Skincare Routine to Prevent Acne
(The Simple Morning and Night Plan I Recommend to My Patients)
If there’s one thing I always tell my acne patients, it’s this:
You do not need a 10-step routine. You need a consistent one that works.
Over the years, I have helped hundreds of people clear their skin by simplifying their skincare — not complicating it. The key is using the right products, in the right order, for your skin type.
Let me share the routine I often recommend — one that you can follow easily, whether your acne is mild or active.
Morning Routine (AM)
You are prepping your skin to stay balanced and protected through the day.
1. Gentle Cleanser
Use a mild, sulfate-free face wash — preferably with salicylic acid if your skin is oily or acne-prone.
2. Toner (Optional)
If your skin feels oily or sweaty after cleansing, use a toner with witch hazel or niacinamide. Avoid alcohol-based toners.
3. Acne Treatment (if prescribed)
Apply a thin layer of any spot treatment — like benzoyl peroxide, adapalene, or clindamycin — only on active breakouts. Let it dry before moving to the next step.
4. Lightweight Moisturizer
Yes, even oily skin needs moisture. Choose an oil-free, non-comedogenic moisturizer with ingredients like hyaluronic acid or ceramides.
5. Sunscreen (Always)
This is non-negotiable. Use a broad-spectrum SPF 30+ daily, even indoors. Look for gel or matte-finish sunscreens if you break out easily.
Evening Routine (PM)
This is when your skin heals and repairs.
1. Double Cleanse (If you wore sunscreen or makeup)
First, use micellar water or a gentle oil cleanser to dissolve buildup. Follow with your regular face wash to clean deeply.
2. Treatment Step
Apply any topical acne treatments as directed by your doctor — like retinoids or azelaic acid. Start with alternate nights if your skin is new to actives.
3. Moisturizer
Lock in hydration with a night-friendly, barrier-supporting moisturizer. If you’re using strong actives, choose one with panthenol, niacinamide, or ceramides.
4. Spot Treatment (if needed)
Only on cysts or stubborn pimples — not your full face. You can use pimple patches or sulfur-based creams overnight.
Weekly Add-Ons (1–2 times/week)
- Gentle exfoliation: A BHA (like salicylic acid) once a week can unclog pores
- Clay mask: Helps absorb oil and soothe inflammation
- Steaming or warm compress: Useful for blackheads or clogged pores — but not for active, inflamed acne
Common Mistakes I Advise Patients to Avoid
- Over-washing or scrubbing too hard — this damages your skin barrier
- Using too many actives at once (retinol + vitamin C + acids = overload)
- Skipping sunscreen while using actives (leads to pigmentation)
- Touching your face or picking pimples
- Sleeping with makeup on
Consistency matters more than fancy products. I’ve seen excellent results from patients who stuck to this simple routine for 6–8 weeks — often better than those who jumped from one product to another.
In the next section, I’ll explain when it is time to stop self-treating and visit a skin doctor — and how a proper consultation can change everything.
When to Visit a Dermatologist
(And Why Waiting Too Long Can Make Things Worse)
Let me tell you about a patient I met a few months ago — a 28-year-old woman named Nisha (name changed for privacy). She had been dealing with acne for over two years. She had tried everything — DIY remedies, drugstore creams, even skipping dairy.
By the time she came to me, she was exhausted — physically and emotionally. Her skin was inflamed, and deep scars were starting to form along her jawline.
Her first question to me was,
“Did I wait too long to get help?”
Sadly, the answer was yes.
You Don’t Need to Wait for a ‘Worst Case’ to Get Medical Help
If your acne is mild and comes and goes, you might be able to manage it with a solid skincare routine and a few lifestyle changes. But if it’s not improving — or if it’s getting worse — please don’t keep trying random fixes.
Here’s what I tell patients to watch out for.
Signs It’s Time to See a Skin Doctor
If you answer “yes” to any of these, it’s time to book a consultation — whether with me or any trusted skincare expert:
- Are your breakouts deep, painful, or cystic?
- Is your acne leaving behind dark spots or permanent-looking marks?
- Have you been treating your acne for 2+ months with no visible improvement?
- Do you feel anxious or embarrassed about your skin in public?
- Are breakouts interfering with your work, dating life, or confidence?
- Does your acne flare up before your period, or with hormonal symptoms like facial hair or hair fall?
- Do you get acne on multiple areas — like your back, chest, and shoulders — not just your face?
What Happens During a Consultation with Me?
I often see nervous first-timers who think they’ll be judged or pushed into laser treatments.
That’s not how I work.
Here’s what usually happens in our first meeting:
- I listen to your full acne history — what you’ve tried, what’s worked, and what hasn’t
- We do a visual skin analysis (sometimes with magnification)
- If needed, I recommend basic blood tests to check hormones or deficiencies
- You leave with a customized skin plan — based on your acne type, skin sensitivity, and goals
And no — I don’t push any unnecessary treatments. You get honest advice. That’s it.
Why Early Treatment Matters
Acne that’s caught and treated early heals faster, causes fewer scars, and often needs milder interventions.
I’ve seen cases where we avoided oral medications or strong peels just because the patient came in early — before things got out of hand.
Getting help for your acne is not vanity. It’s healthcare.
In the next section, I’ll walk you through how to stop pimples from coming back repeatedly — by building simple, long-term habits.
How to Stop Pimples from Coming on Face
(Simple Habits I Teach My Patients That Actually Work)
When someone asks me,
“Doctor, how do I stop these pimples from coming again and again?”
I always say this: You don’t treat acne once and forget about it. You manage it like your health.
And just like health, clear skin starts with habits — not miracles.
Over the years, I’ve seen the best results in patients who focus less on aggressive treatment and more on smart, consistent prevention.
Here’s what I recommend to keep breakouts from returning.
1. Cleanse Smart, Not Hard
- Wash your face twice a day — no more, no less
- Use a mild, non-drying face wash (especially if you’re using actives like retinoids)
- After workouts or sweating, rinse with lukewarm water — not cold or very hot
Over-cleansing strips your skin and leads to rebound oiliness.
2. Treat Early — Don’t Wait for Full-Blown Breakouts
- Feel a pimple forming? Dab a thin layer of benzoyl peroxide or salicylic acid immediately
- Use pimple patches overnight for isolated breakouts
- Do not squeeze or poke — this spreads bacteria and leaves marks
Treating early stops acne from becoming inflamed and painful.
3. Moisturize and Protect (Even Oily Skin Needs It)
- Always use a lightweight, non-comedogenic moisturizer
- Never skip sunscreen — especially when using acne treatments
- At night, apply your topical medications before moisturizer if directed — unless skin is too dry
Moisture keeps your skin barrier strong and resistant to flare-ups.
4. Watch Your Hands — and Your Triggers
- Avoid touching your face throughout the day
- Clean your phone screen and pillowcases regularly
- Be mindful of triggers like:
- Period cycle
- Exam or work stress
- Sleep changes
- Diet slip-ups (like sudden junk food binges or whey protein)
Acne often reflects lifestyle shifts. Recognize patterns early.
5. Keep Your Stress and Sleep in Check
This one is underrated.
When my patients fix their sleep and reduce emotional burnout, their skin starts healing — often faster than expected.
Try:
- Sleeping at the same time every night (7–8 hours minimum)
- Deep breathing or 10 minutes of meditation daily
- Reducing screen time before bed
- Avoiding caffeine late in the evening
- Your hormones and immunity work best when your mind is calm.
6. Follow the 3-Week Rule Before Quitting Products
One mistake I often see is switching products too quickly.
- Skin takes 3–6 weeks to respond to any new treatment
- Initial purging is normal with retinoids and exfoliants
- Stick to one change at a time so you know what’s working
- Be patient. Skincare is not an overnight fix.
Bonus: Customize Your Routine — Don’t Copy Others
Just because a serum worked for your friend does not mean it will work for you.
That is why I always assess acne based on skin type, triggers, and response to ingredients — not just product names.
When you treat your skin with consistency, gentleness, and awareness — it rewards you with clarity and balance.
And remember, prevention is not about perfection — it is about staying one step ahead of your triggers. In the next section, I’ll answer the most common acne-related questions I hear in my clinic — including some myths people still believe.
Conclusion
(Clear Skin Starts with the Right Approach)
If you’ve made it this far, I want to thank you for taking the time to truly understand your skin.
Acne is not just a cosmetic concern — it affects how you feel about yourself. And I’ve seen how the right treatment, started at the right time, can completely change lives.
This guide walked you through the acne causes, symptoms, treatment options, and deeper triggers that many people overlook.
Remember, there is no single solution that works for everyone. Your skin needs care, patience, and the right guidance.
If you are dealing with stubborn acne, do not wait too long. The earlier you take action, the easier it is to prevent scarring and long-term damage.
I hope this guide helped you take that first step.
Looking for the Best Acne Treatment in Delhi?
If you are searching for a trusted acne specialist in Delhi — especially around South Delhi, CR Park, or Alaknanda — I offer personalized acne consultations at Care Well Medical Centre.
Whether it’s teenage acne, hormonal breakouts, or stubborn acne scars, we will create a treatment plan that works specifically for your skin and lifestyle.
Visit Us:
Care Well Medical Centre
House No. 1, NRI Complex, Chittaranjan Park (C.R.Park), NRI Colony, Mandakini Enclave Colony, Alaknanda, New Delhi, Delhi 110019
🌐 www.carewellmedicalcentre.com
Call Us:
Book Appointment:
Acne FAQs (Frequently Asked Questions)
(Honest Answers to the Most Common Doubts I Hear Every Day)
I often say — half the battle with acne is knowledge. When you understand what is true (and what is not), you stop wasting time and energy on the wrong things.
Here are some of the most frequent questions my patients ask — along with what I tell them.
No — and anyone who promises that is misleading you. Some home remedies may reduce redness quickly, but acne is a chronic skin issue. It needs consistency and a 4–6 week plan, minimum. Quick fixes often lead to more damage.
Not directly.
Cocoa is not the problem — sugar and dairy in commercial chocolate are. If you are sensitive, high-sugar or milk-based chocolates may trigger breakouts. Dark chocolate (80% or above) is usually safe in moderation.
No.
Acne is not a hygiene issue. In fact, over-washing or scrubbing can worsen it. Acne forms due to oil, bacteria, hormones, and inflammation beneath the skin — not from surface dirt.
Yes — and I see this often.
Dandruff (seborrheic dermatitis) flakes can block pores on the forehead. Hair oils and unwashed scalp buildup also contribute. Treating the scalp often helps clear the skin.
Yes.
Teen acne is usually due to puberty and excess oil. Adult acne — especially in women — is often hormonal, stress-related, or triggered by lifestyle changes. It tends to show up around the chin and jawline.
No, this is a myth.
There is no scientific link between masturbation and acne. Acne is hormonal, but not in the way most people assume. Do not blame normal biology.
Some do.
Red or brown marks (called PIH) usually fade with time and sunscreen. But deep scars — like icepick or boxcar scars — need professional treatments like microneedling, laser, or chemical peels. The earlier you treat active acne, the less scarring you risk.
It depends.
Using heavy, comedogenic (pore-clogging) makeup — especially without proper removal — can aggravate breakouts. But non-comedogenic, breathable makeup used with proper cleansing is safe for acne-prone skin.
Possibly.
Some patterns do suggest a link between digestive inflammation and skin issues, especially on the cheeks or temples. If you have both bloating and breakouts, improving gut health might help.
I usually advise against it.
Most natural oils are comedogenic, meaning they can clog pores and worsen acne — especially coconut oil. Acne-prone skin needs lighter hydration — like squalane, rosehip, or aloe-based gels.
If you have more questions, know this: you are not alone. Every skin is different, and every case of acne deserves personal care — not just generic advice.
📚 References:
- National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS).
“Acne: Overview, Diagnosis, and Management.”
Available at: https://www.niams.nih.gov/health-topics/acne - Zaenglein AL, et al.
“Guidelines of care for the management of acne vulgaris.” Journal of the American Academy of Dermatology.
Available at: https://pubmed.ncbi.nlm.nih.gov/26897386/ - Mayo Clinic.
“Acne: Symptoms and Causes.”
Available at: https://www.mayoclinic.org/diseases-conditions/acne/symptoms-causes/syc-20368047 - Thiboutot D, et al.
“Acne pathogenesis and updated treatment options.” National Library of Medicine (NCBI).
Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7275854/ - American Academy of Dermatology (AAD).
“How Dermatologists Treat Acne.”
Available at: https://www.aad.org/public/diseases/acne/derm-treat