As a cosmetic surgeon practicing in Delhi for over 15 years, I often meet women who want clear, factual information about hymenoplasty—without judgment or social pressure. Many women ask what hymenoplasty surgery actually means from a medical perspective, and I see it as my responsibility to explain the facts calmly and honestly.
Hymenoplasty is a minor surgical procedure that repairs or reconstructs hymenal tissue at the vaginal opening. I perform this procedure as a daycare surgery under local or general anesthesia, and it typically takes 30–45 minutes. Virginity is not a medical concept, and this procedure addresses only a physical concern—it does not change your history, your value, or who you are as a person.
This article offers judgment-free, evidence-based information on hymenoplasty, including medical facts, common myths, safety, recovery, timing, and how to find a qualified surgeon in Delhi. I maintain strict confidentiality for all consultations and medical records under patient–doctor privilege.
What Is Hymenoplasty Surgery?
Hymenoplasty surgery is a minor cosmetic gynecological procedure that repairs or reconstructs hymenal tissue at the vaginal opening. As a surgeon, I perform this procedure to address anatomical concerns, not to change sexual history or personal identity.
When patients ask what hymenoplasty surgery involves, I explain that it falls under cosmetic gynecology—procedures that address physical appearance or structure rather than treating disease. I recommend it only after a detailed consultation, where I assess your anatomy, general health, and expectations. The aim is always to offer a safe and medically appropriate option, not to reinforce social myths or pressure.
What hymenoplasty can do
- Reconstruct or repair hymenal tissue at the vaginal opening
- Restore the physical appearance of the hymen
- Provide a medically safe option when desired
What hymenoplasty cannot do
- Restore or define virginity
- Tighten the vagina
- Change sexual history, fertility, hormones, or menstruation
- Guarantee bleeding during future intercourse
The most important point to remember is that restoring virginity is not a medical goal of hymenoplasty. Virginity has no medical definition. As a doctor, my responsibility is to provide clarity, safety, and realistic expectations—so that any decision you make remains informed and free from pressure.
What Is the Hymen? Medical Facts You Should Know
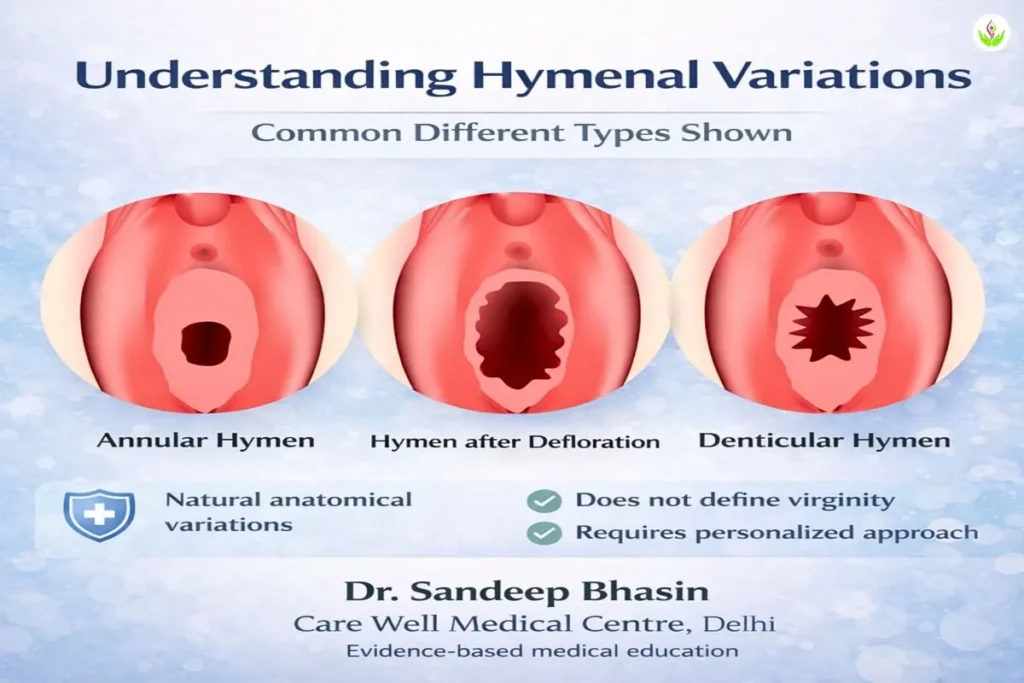
If you are wondering what the hymen is medically, it is a thin, elastic fold of tissue located at the entrance of the vagina. It is present from birth, but its shape, thickness, and elasticity vary widely from one woman to another.
In my clinical practice, I see many normal variations, and no single hymen type defines health, sexuality, or identity.
Natural variations are common
Medically, the hymen can appear in different forms—crescent-shaped, ring-like, or with small openings. In some women, it is very elastic; in others, it is minimal or naturally absent from birth. These differences are completely normal. Because of this variation, the hymen may stretch rather than tear, even during activities that place pressure on the vaginal opening.
No proven protective function
There is no scientific evidence that the hymen serves a protective role against infection. This myth likely arose from cultural beliefs rather than medical science. Vaginal health depends on internal factors such as natural flora and immunity, not on the presence or absence of the hymen. This is an important medical distinction, as many social beliefs incorrectly assign functions to this tissue.
Bleeding is not a reliable indicator
A key point I always clarify is that the presence or absence of bleeding during first intercourse has no reliable correlation with the hymen’s condition. Many women do not bleed during first intercourse, while some may experience spotting due to vaginal dryness or minor tissue friction. Bleeding is therefore not a medical marker of virginity or sexual activity.
Understanding these facts helps separate medical reality from social myths, allowing you to approach the topic of hymenoplasty with clarity rather than fear or misinformation.
What Causes the Hymen to Tear Without Sexual Activity?
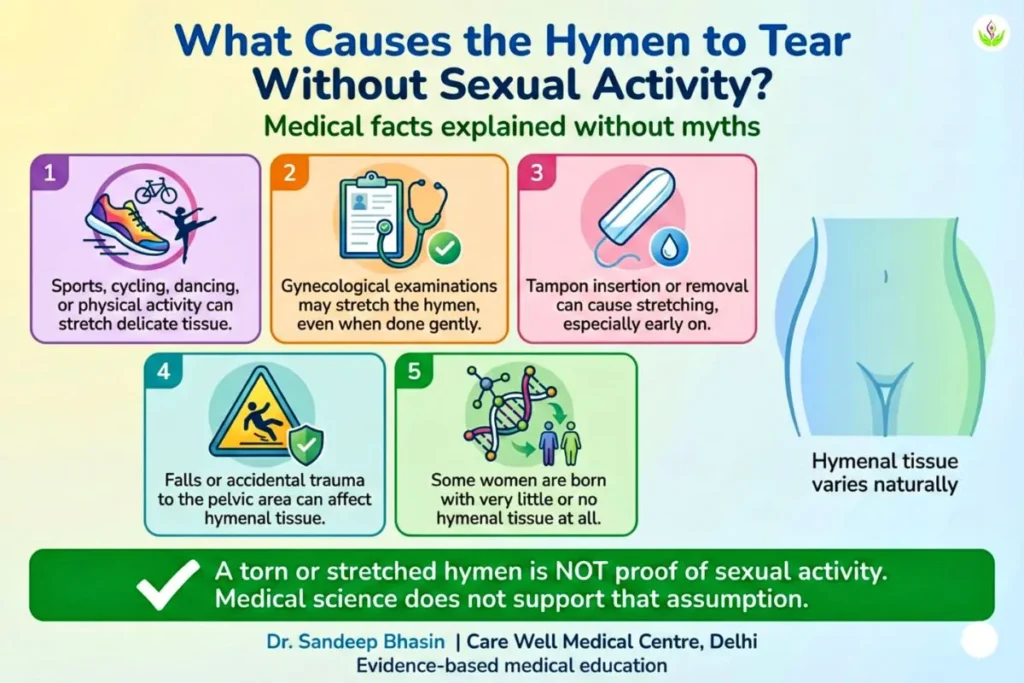
In my practice, one of the most common misunderstandings I encounter is the belief that a torn hymen always indicates sexual activity. Patients often ask what causes the hymen to tear without sexual activity, and medically, the answer is clear: the hymen is a delicate and highly variable tissue that can stretch or tear due to several non-sexual, everyday reasons.
Common non-sexual causes include
- Sports, cycling, and dancing: Activities involving repetitive movement, stretching, or pressure around the pelvic area can stretch or tear the hymen, especially if it is thin or less elastic.
- Medical examinations: Gynecological exams or procedures may stretch the hymen, even when performed gently and correctly.
- Tampon use: Inserting or removing tampons can stretch or tear hymenal tissue, particularly during early use.
- Accidental injury: Falls, slips, or trauma to the pelvic area can affect the hymen unintentionally.
- Natural absence: Some women are born with very little hymenal tissue or none at all, which is a normal anatomical variation.
Because of these factors, many women may have a stretched or torn hymen long before any sexual activity, while others may retain hymenal tissue even after intercourse.
The most important reassurance I give patients is this: a torn hymen is not proof of sexual history. Medical science does not support that assumption. Understanding this helps reduce unnecessary anxiety and ensures that any decision about hymenoplasty is based on medical facts, not social myths.
Can Hymenoplasty Restore Virginity?
Patients often ask whether hymenoplasty can restore virginity. The medical answer is no, because medicine does not define virginity. The medical answer is no, because virginity is not a medical concept.
Medicine does not define morality, purity, or personal history. These ideas come from social and cultural beliefs, not from biology. As a doctor, my responsibility is to explain what medicine can and cannot do, without reinforcing pressure or myths.
Hymenoplasty has one medical role only—it reconstructs or repairs hymenal tissue at the vaginal opening. It does not reverse life events, erase past experiences, or redefine who you are. Clinically, this procedure addresses tissue anatomy only.
It is also important to understand that hymenoplasty does not guarantee bleeding during future intercourse. Many women with a natural hymen do not bleed, and bleeding itself is not a reliable medical outcome.
To be ethically clear: there are no promises and no moral framing in hymenoplasty. Any decision should be based on medical facts and personal choice, not fear, guilt, or social myths.
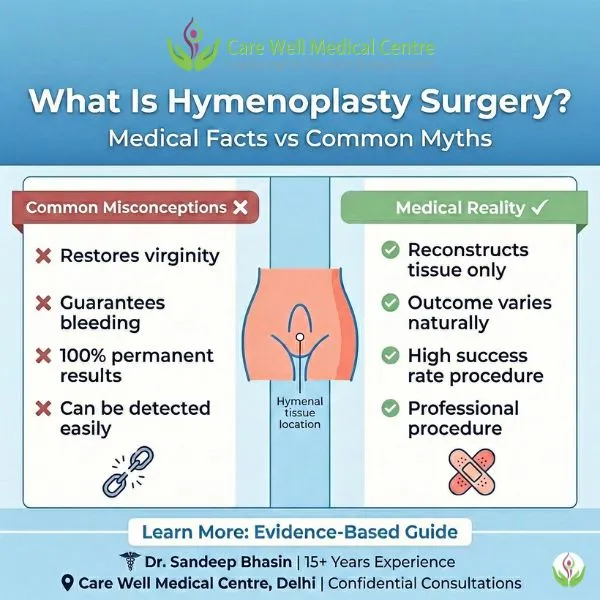
Common Misconceptions About Hymenoplasty Surgery
In my practice, I find that most anxiety around hymenoplasty comes from misinformation, not from the procedure itself. Let me address the most common misconceptions calmly and clearly, using medical facts rather than social assumptions.
Myth: Hymenoplasty restores virginity
Medical reality: Virginity is not a medical concept. Hymenoplasty reconstructs hymenal tissue only. It cannot change life history, personal experiences, or identity.
Myth: Hymenoplasty Always Causes Bleeding
Medical reality: No surgery can guarantee bleeding. Many women with a natural hymen do not bleed, and some may experience spotting due to dryness or friction. Bleeding is not a reliable medical outcome.
Myth: Your partner will never know
Medical reality: Medicine does not offer guarantees about what someone may or may not notice. Physical responses vary widely. Surgery cannot control perception or relationships.
Myth: Hymenoplasty tightens the vagina
Medical reality: Hymenoplasty does not tighten the vagina. It involves only superficial tissue at the vaginal opening and does not affect vaginal muscles or sexual function.
Myth: Hymenoplasty Can Be Repeated Multiple Times
Medical reality: Hymenal tissue is limited. Repeated surgeries are not always possible or advisable and depend on individual anatomy and healing.
Myth: Results are always permanent
Medical reality: Results may change with physical activity, injury, or time. As with any tissue repair, outcomes vary from person to person.
The key takeaway is simple: hymenoplasty is a medical procedure with defined limits. Understanding these realities helps you make decisions based on facts, not fear or expectations created by myths.
When Do Doctors Consider Hymenoplasty Medically Appropriate?
As a doctor, I consider hymenoplasty medically appropriate only under specific, well-defined conditions. This decision is never casual and never automatic. My primary role is not to approve or deny a request blindly, but to protect you from pressure, misinformation, or coercion while ensuring medical safety.
Age eligibility
I consider hymenoplasty only for adults above 18 years of age. This ensures legal validity, personal maturity, and the ability to provide independent consent. I do not recommend or perform this procedure for minors under any circumstances.
Informed consent
Informed consent is essential. This means you clearly understand:
- What the procedure can do
- What it cannot do
- Possible risks and limitations
- Realistic outcomes
Consent must come from you alone, without influence from family members, partners, or external expectations.
Mental and emotional readiness
Medical appropriateness includes emotional readiness. I take time to assess whether you are making this decision calmly and voluntarily. If I sense distress, fear, or emotional pressure driving the request, I pause and counsel first. Surgery should never be used as a response to anxiety or guilt.
No coercion—ever
I do not consider hymenoplasty appropriate if there is any form of coercion. This includes pressure related to marriage, relationships, family demands, or social threats. A doctor’s responsibility is to act as a safeguard, not as a facilitator of force or fear.
Medical evaluation matters
Before proceeding, I perform a proper medical evaluation, which includes:
- General health assessment
- Gynecological examination (only if necessary and with consent)
- Review of medications and medical history
This step ensures safety and helps determine whether surgery is technically feasible and medically reasonable.
The most important principle I follow is this:
a doctor’s role is to protect patients from pressure, not to reinforce it. Doctors consider hymenoplasty appropriate only when it aligns with medical ethics, patient autonomy, and informed choice.
Why Do Women Consider Hymenoplasty in India?
In India, women often ask about hymenoplasty because of social and personal pressures rather than medical necessity. Understanding these reasons helps explain the context, without endorsing the beliefs behind them.
- Cultural expectations: Some communities wrongly associate an intact hymen with purity or virtue. These are cultural beliefs, not medical facts, but they can still create emotional pressure.
- Marriage-related anxiety: Fear of judgment before or after marriage is a common concern, especially due to misconceptions about bleeding or “proof” of virginity.
- Personal reasons: Some women consider hymenoplasty for private, personal reasons related to self-perception or emotional readiness. These choices should always be voluntary and informed.
- Trauma survivors: A small but important group includes women who have experienced sexual trauma. This requires a sensitive, patient-led approach. Surgery is not a treatment for trauma itself.
Medical ethics ensure complete privacy and confidentiality. All consultations, examinations, and medical records remain strictly protected under patient–doctor privilege.
This context explains why women inquire about hymenoplasty in India, while medical decisions continue to follow ethical and safety standards.
How Doctors Perform Hymenoplasty Surgery?
I perform hymenoplasty as a short daycare procedure, and patients often ask how the surgery works. The process is usually simpler than most expect. My goal is always to reduce anxiety by explaining the steps clearly, without unnecessary technical detail.
I perform the procedure under local or general anesthesia, depending on individual comfort and medical suitability. This ensures that you do not feel pain during the surgery. In most cases, the procedure takes approximately 30 to 45 minutes, and you can return home the same day after a brief period of observation.
From a surgical standpoint, hymenoplasty involves delicate reconstruction of the thin tissue layer at the vaginal opening. There are no visible external scars, and the stitches used are typically absorbable, so they do not require removal.
We treat confidentiality as the highest priority. From registration to discharge, we manage every aspect of care discreetly and professionally, in strict accordance with patient–doctor confidentiality. We do not share any information without your explicit consent.
I provide this overview to help you understand the procedure with confidence. I always discuss detailed planning, safety protocols, and aftercare instructions privately during your personal consultation.
What Is Hymenoplasty Surgery? (Video Explanation)
Some patients prefer a visual explanation to better understand medical procedures. In this short video, I explain what hymenoplasty surgery is, how it is performed, and what patients can realistically expect—using simple, non-graphic, and medically accurate language.
This video is meant to reduce anxiety and clear common doubts about safety, pain, confidentiality, and recovery. It complements the written explanation above and reflects the same ethical, evidence-based approach discussed throughout this article.
What Is the Recovery Process Like After Hymenoplasty?
Recovery after hymenoplasty is usually smooth and predictable, especially when basic aftercare instructions are followed. I explain recovery in practical terms so you know what to expect day by day, without unnecessary worry.
Doctors discharge most patients the same day after a short observation period. Patients usually experience only mild discomfort or soreness rather than sharp pain, and prescribed medication controls it well.
Activity timeline (general guidance)
- Walking: You can walk immediately after the procedure. Gentle movement is encouraged.
- Work and daily routine: Most patients return to desk work or normal activities within 1–2 days.
- Exercise and strenuous activity: Avoid gym workouts, running, cycling, or heavy lifting for 3–4 weeks to allow proper healing.
- Sexual activity: From a medical standpoint, intercourse is usually advised after about 6 weeks, once healing is complete.
Hygiene and wound care
I advise keeping the area clean and dry. Gentle washing with water is sufficient; harsh soaps, vaginal douching, or internal products should be avoided during healing. Proper hygiene significantly reduces the risk of infection.
Stitches and healing
The stitches used are dissolvable, so they do not need to be removed. Healing progresses gradually over a few weeks, and most patients do not notice anything unusual during this phase.
Follow-up matters
A follow-up visit is important to ensure healing is on track and to address any concerns early. This is part of responsible medical care, not a formality.
The key reassurance I give all patients is this: there are no visible external changes after recovery. Healing occurs internally, and day-to-day appearance remains unchanged.
Overall, recovery is quiet, discreet, and manageable, and most patients resume normal life quickly with proper guidance.
When Should You Plan Hymenoplasty Surgery? (Timing Matters)
Proper timing helps ensure safer healing and less emotional stress. In my experience, when hymenoplasty is planned calmly rather than rushed, recovery is smoother and concerns are fewer.
One of the most common questions I receive is: when should hymenoplasty surgery be scheduled? Medically, the general guideline is 4–6 weeks before anticipated sexual activity. This timeframe allows adequate tissue healing and reduces the risk of discomfort or delayed recovery.
Why planning ahead matters
- Allows complete healing of delicate tissue before physical activity
- Reduces stress caused by last-minute decision-making
- Provides buffer time for any unexpected delays or individual healing differences
Timing considerations
Menstrual cycle: I advise avoiding surgery during menstruation. Scheduling the procedure soon after your period ends is usually more comfortable and hygienic.
Wedding season planning: In Delhi, peak wedding months typically fall between November and February. If surgery is being considered around a wedding, early consultation helps avoid rushed decisions close to important life events.
Allowing a safety buffer
Although recovery is usually straightforward, healing varies from person to person. Keeping extra buffer time supports both physical comfort and emotional readiness.
The guiding principle is simple: adequate planning protects your recovery and your peace of mind. My role is to help you choose a timeline that fits your individual situation safely and responsibly.
Does Hymenoplasty Guarantee Bleeding After Intercourse?
One of the most important questions patients ask is: does hymenoplasty guarantee bleeding after intercourse? The clear medical answer is no. Hymenoplasty does not guarantee bleeding during intercourse.
Even women with a natural hymen may not bleed at all. When bleeding does occur, it is often related to factors such as tissue elasticity, vaginal dryness, or friction—not to whether the hymen is natural or reconstructed.
A reconstructed hymen behaves much like natural tissue. It may stretch without tearing, or there may be mild spotting. Because of normal biological variation, bleeding is not a reliable marker of success.
I always explain this clearly: hymenoplasty is a procedure to reconstruct tissue, not to produce a specific outcome. Results vary from person to person. Some women may experience light spotting, others may not bleed at all—and both outcomes are medically normal. Expectations should be based on medical facts, not social myths.
Risks and Safety: Is Hymenoplasty Medically Safe?
In my clinical practice as a cosmetic surgeon, I evaluate hymenoplasty with the same safety standards as any other surgical procedure. When performed by a qualified doctor under proper medical conditions, hymenoplasty is generally safe, but it must never be treated casually.
When hymenoplasty is considered medically safe
Based on clinical guidelines and experience, safety depends on:
- Proper medical evaluation before surgery
- Performance by a trained and experienced surgeon
- A sterile operating environment
- Clear, informed consent after explaining limits and risks
- Availability of follow-up care
Possible medical risks
From a medical standpoint, most patients recover without complications. However, possible risks include:
- Mild bleeding or spotting in the first few days
- Temporary swelling or discomfort
- Infection (rare when hygiene and instructions are followed)
- Delayed healing in some individuals
These risks are usually minor and manageable with timely care.
When hymenoplasty is not advisable
I do not consider hymenoplasty appropriate if there is:
- An active vaginal or pelvic infection
- Uncontrolled diabetes or blood-clotting disorders
- A history of poor wound healing
- Emotional distress, fear, or pressure influencing the decision
The most important safety consideration
In my experience, the greatest risk is not surgical—it is unrealistic expectation. Hymenoplasty has clear medical limits. Understanding what the procedure can and cannot do is essential for both physical safety and emotional wellbeing.
As a doctor, my responsibility is to prioritise patient safety, autonomy, and ethical care, not to make promises or reinforce social pressure.
Finding a Qualified Hymenoplasty Surgeon in Delhi
Choosing the right surgeon is as important as the procedure itself. In my experience, most dissatisfaction and anxiety arise not from hymenoplasty, but from poor counselling, unrealistic promises, or lack of privacy. This section is meant to help you make a safe, informed decision.
With over 15 years of experience practicing in Delhi, including focused work in cosmetic gynecology and hymenoplasty, I clearly understand what patients should look for—and which warning signs they should never ignore.
What to look for in a surgeon and clinic
- Relevant experience in cosmetic gynecology: Hymenoplasty involves delicate tissue reconstruction. Surgeons without specific experience in this area may lack the required precision.
- Strict privacy protocols: Confidentiality should apply to consultations, medical records, billing, and all communication—not just the surgery itself.
- Accredited medical facility: A licensed clinic with proper sterilisation, anesthesia support, and emergency readiness is essential for patient safety.
Red flags you should avoid
- Guarantees of bleeding or “100% results”: These claims are medically dishonest.
- Pressure tactics: Rushing decisions, linking surgery to marriage timelines, or using fear-based counselling.
- Unusually low pricing: This can indicate compromised safety standards, inadequate facilities, or inexperience.
Questions you should ask during consultation
- How many hymenoplasty procedures have you performed?
- What outcomes and limitations should I realistically expect in my case?
- What privacy measures do you follow for records and communication?
- Who will support me if I have concerns after the procedure?
Ready to take the next step?
If you would like personalised guidance, you can book a confidential hymenoplasty consultation in Delhi to understand the procedure, safety considerations, expected recovery, and cost details in a private, judgment-free setting.
Confidentiality you can rely on
Medical ethics require complete confidentiality. From consultation to surgery to follow-up, your information must remain private and is never shared without your explicit consent.
Making the right choice protects not only your physical safety, but also your dignity and peace of mind.
Key Takeaways for Patients
- Hymenoplasty is a minor surgical procedure that reconstructs or repairs hymenal tissue at the vaginal opening. It addresses a physical concern only and is performed under proper medical care.
- Virginity is not a medical concept. No surgery can restore or define virginity, personal history, or identity.
- When done by a qualified doctor, hymenoplasty is generally safe, provided proper evaluation, ethical practice, and follow-up care are in place.
- Bleeding is not guaranteed after hymenoplasty or even with a natural hymen. Bleeding is not a reliable marker of success.
- Choosing hymenoplasty is a personal decision, not a moral obligation. It should always be voluntary, informed, and free from pressure.
- A confidential consultation with an experienced surgeon is essential to understand realistic outcomes, safety considerations, and whether the procedure is appropriate for you.
Hymenoplasty Surgery FAQs – Medical Answers You Can Trust
No. A torn or stretched hymen is not proof of sexual activity. Sports, cycling, tampon use, medical examinations, accidental injury, or natural anatomy can all affect the hymen. Medical science does not use the hymen to determine sexual history.
Yes. Hymenoplasty surgery is completely confidential under patient–doctor privilege. Consultations, medical records, billing, and follow-ups are handled discreetly. No information is shared without your explicit consent.
No. Hymenoplasty involves only superficial tissue at the vaginal opening. It does not affect fertility, pregnancy, childbirth, menstruation, or routine gynecological examinations.
No. Hymenoplasty does not guarantee bleeding. Even women with a natural hymen may not bleed. Bleeding varies due to tissue elasticity, dryness, and individual anatomy and is not a medical success marker.
In most cases, after proper healing, a reconstructed hymen cannot be easily distinguished from natural tissue during routine examination. However, medicine does not offer absolute guarantees, and detection is not the purpose of the procedure.
I usually complete the procedure in 30–45 minutes as a daycare surgery and discharge most patients the same day, typically within 2–3 hours, after a short observation period.
In Delhi, hymenoplasty surgery generally costs ₹25,000 to ₹50,000. The final cost depends on surgeon experience, facility standards, anesthesia, and individual medical needs. Exact pricing is discussed during a confidential consultation.
✔ ️ All medical information reviewed and verified by Dr. Sandeep Bhasin, Senior Cosmetic Surgeon, Delhi.
Medical Disclaimer & Author Verification
Medical Disclaimer:
This article is intended for educational purposes only. It does not replace a personal medical consultation, diagnosis, or treatment plan. Individual results and recovery experiences vary based on age, anatomy, medical history, and overall health. Any medical decision should be made after a direct consultation with a qualified doctor.
Author Verification:
All medical information in this article has been reviewed and verified by Dr. Sandeep Bhasin, Senior Cosmetic Surgeon.
Clinical Practice:
Care Well Medical Centre, Delhi
Last medically reviewed: February 2026